Over 30 years ago, as a brand-new graduate nurse, I was starry-eyed and ready to change the world – one patient’s life at a time.
Over time, I discovered that my passion to make a difference paired with my ability to communicate and connect with others could work well in other avenues of healthcare such as quality, patient safety, and regulatory.
I wanted to facilitate processes that made it as easy as possible for every healthcare professional to do the right thing for every single patient every single time.
However, sometimes the best intentions may backfire and may even make it more difficult for the patient care frontline to do their jobs – particularly if initiatives outlive the problem they were designed to solve.

Let me explain, pre-pandemic there were more nurses and more time for them to participate in performance improvement projects and influence the practice changes that impacted their every day. Checklists and audits created healthy reminders of steps toward best evidenced-based practice.
But then the whole world, and in particular our healthcare world, was changed by that invisible-to-the-naked-eye enemy. COVID-19. We were already on shaky ground with new nurses not being educated quickly enough to replace retiring ones and high rates of burnout during the best of times. But now as many as 1 in 5 fulltime healthcare professionals are leaving those roles. Suicide rates among healthcare professionals – which were never low – are now higher than ever.
So, actions like asking a charge nurse to complete daily audits or pulling a nurse manager into multiple performance improvement actives may have worked a few years ago. But asking those same things now when charge nurses and managers are often pulled into staffing with full patient loads doesn’t feel like supporting them anymore.
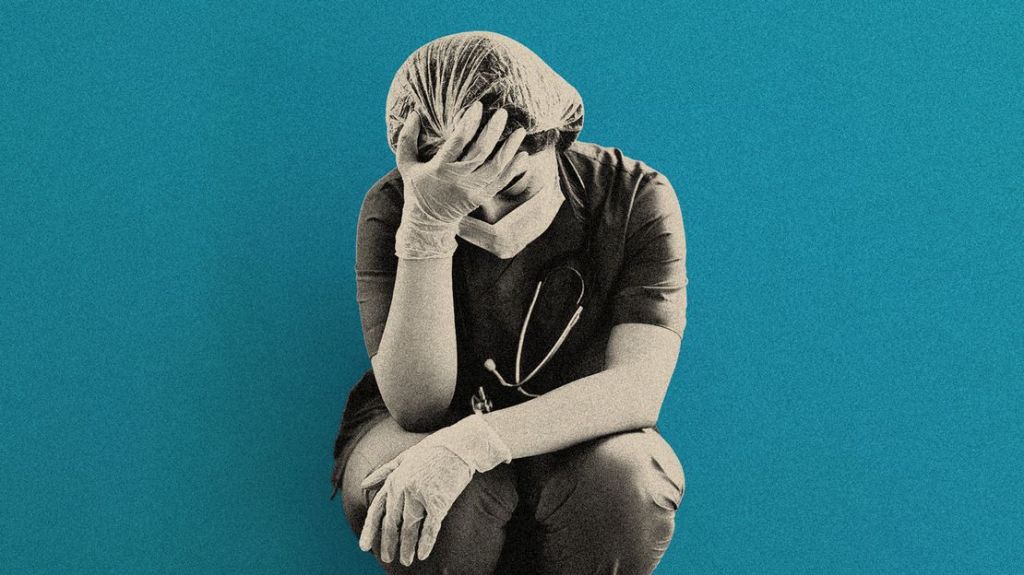
I absolutely know that processes in healthcare need to be checked and audited. But I also know that throwing one more thing on already stretched – sometimes traumatized even – healthcare team members can be that “final straw” that causes them to call it quits.
For me, personally, I am coming full circle in my career and actually taking a career break in order to regroup and find ways to wear scrubs more and carry “corrective clipboards” less. (Plus, this break coincides will with my taking some long overdue time for some healing and processing of a couple strong blows that have hit my personal life hard in recent years). I know not everyone has the ability to do this, but I believe there are some things everyone in healthcare leadership can easily do to be a blessing-not-a-burden, asset-not-an-a$$-kicker, supporter-not-a-destroyer, and an encourager-not-an-enforcer. (You get the idea).

- Wear scrubs
- Sometimes it’s as simple as losing the polyester power suit or dress and being a little more relatable
- Jump in and do something tangible for them!
- You may be like me and it’s been a minute since your clinical days. It may not be safe for you to take a whole load of patients. But if you’re more on the administrative side of health care these days, even taken 10-15 minutes out of your day to answer phones or call lights or calm a confused patients could make the difference and make you much easier to listen to when you give them correction or advice.
- Uplift more than you correct.
- Remember when all the leadership gurus were touting the importance of sandwiching correction or any other information that may weigh someone down between positive/uplifting comments? Well, that is more important than ever!
Just being present and listening can mean more than you ever know. Now more than ever, healthcare professionals may feel warn and torn – like a ragamuffin. If they see your heart, time, and intention – you may be just the oasis a weary soul needs.




